monkeypox
How to Prevent and Treat Mpox
Mpox, previously known as monkeypox, is a rare viral disease caused by the mpox virus. Although it was initially found in Central and West Africa, the disease has spread to other parts of the world, due to factors like international travel and close contact with infected individuals. With the outbreak of mpox in 2022, it's more important than ever to understand how to prevent and treat this illness. Let’s learn about the most effective ways to prevent and treat mpox.
What Is Mpox?
Mpox is a zoonotic disease, meaning it can spread from animals to humans. It is caused by the mpox virus, which typically affects rodents and non-human primates. The disease is similar to smallpox but usually less severe.
Mpox is characterized by a fever, rash, and swollen lymph nodes, with symptoms lasting 2 to 4 weeks. The disease can be severe, leading to complications such as severe scarring, blindness, and even death in rare cases.
How Does Mpox Spread?
Mpox spreads through close contact with an infected person or animal. It can also spread through handling materials like bedding or clothing contaminated with the virus. The virus can be transmitted from person to person through:
- Direct contact with an infected person's rash, scabs, or body fluids.- Extended close contact with respiratory droplets, including sexual contact.- Contact with contaminated objects, such as clothes or blankets.
Read more: What is Mpox? How does it affect people?
How to Prevent Mpox
Prevention is key to controlling the spread of mpox. By taking the following steps, you can reduce your risk of infection:
Avoid Close Contact with Infected Individuals
If you know someone who has been diagnosed with mpox, avoid close physical contact with them until they have fully recovered. Mpox is most contagious when the infected person shows symptoms, particularly when they have a rash.
Use Protective Measures
If you must be in contact with someone who has mpox, wear personal protective equipment (PPE) such as gloves, masks, and gowns. This is especially important for healthcare workers and those caring for infected individuals at home.
Practice Good Hygiene
Wash your hands frequently with soap and water, especially after coming into contact with an infected person or animal. If soap and water are not available, use an alcohol-based hand sanitizer.
Avoid Contact with Potentially Infected Animals
Mpox can also spread from animals to humans. Avoid contact with animals that may carry the virus, such as rodents or non-human primates. Do not handle or consume wild game that may be infected, and avoid contact with animal products, such as furs, that could be contaminated.
Disinfect Contaminated Items
If you have been in contact with an infected person or animal, disinfect any objects or surfaces that may have been contaminated. Use a bleach solution or other disinfectant to clean clothing, bedding, and other items.
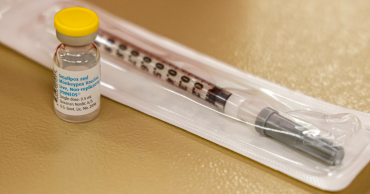
Get Vaccinated
Vaccination is one of the most effective ways to prevent mpox. The smallpox vaccines, such as ACAM2000 and Jynneos, have been shown to protect against mpox because of the close relationship between the smallpox and mpox viruses.
The Centers for Disease Control and Prevention (CDC) recommends vaccination for those who have been exposed to pox or are at high risk of exposure.
Isolate Infected Individuals
If someone in your household has mpox, isolate them in a separate room to prevent the virus from spreading to others. Ensure they use separate bathroom facilities if possible, and do not share personal items like towels or bedding.
Practice Safe Sex
Since mpox can spread through sexual contact, it's important to practice safe sex, especially if you or your partner have been exposed to the virus. Use condoms and dental dams to reduce the risk of transmission.
Read more: Mpox: Common Signs and Symptoms
How to Treat Mpox
While there is no specific cure for mpox, the disease is usually self-limiting, meaning it resolves on its own with proper care. Treatment focuses on relieving symptoms and preventing complications.
Symptom Management
The primary goal of treatment is to manage the symptoms of mpox. This includes:
Pain Relief: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help reduce fever and alleviate pain.Skin Care: The mpox rash can be itchy and uncomfortable. Taking oatmeal baths can help soothe the skin and reduce itching. Applying topical treatments recommended by a healthcare provider can also help.Hydration: Drinking plenty of fluids is essential to prevent dehydration, especially if you have a fever. Staying hydrated also helps keep your skin healthy as it heals from the rash.
Isolation and Rest
If you have mpox, it's crucial to isolate yourself from others to prevent spreading the virus. Stay home, rest, and avoid contact with other people and pets until all lesions have healed. Cover any open sores with bandages or gauze to prevent the spread of the virus.
Antiviral Medications
In severe cases, or for individuals with weakened immune systems, healthcare providers may prescribe antiviral medications like tecovirimat (TPOXX) or cidofovir. These medications are approved for treating smallpox and may be effective against mpox, but more research is needed to confirm their efficacy.
Preventing Secondary Infections
Mpox can lead to secondary bacterial infections, especially if the skin is broken due to scratching. If a secondary infection develops, your healthcare provider may prescribe antibiotics to prevent further complications.
Monitoring and Support
If you have been diagnosed with mpox, your healthcare provider will monitor your condition and provide support as needed. This may include regular check-ins to ensure your symptoms are improving and to address any complications that may arise.
Immune Globulin Therapy
For individuals who are unlikely to respond to the vaccine or antiviral treatments, healthcare providers may consider using vaccinia immune globulin (VIG), which contains antibodies from people who have received the smallpox vaccine. This therapy can help boost the immune system's response to the virus.
Conclusion
Mpox is a serious disease that requires careful attention to prevention and treatment. By understanding how the virus spreads and taking steps to protect yourself and others, you can reduce the risk of infection.
If you do contract mpox, focusing on symptom management and isolation can help you recover safely. Stay informed, practice good hygiene, and consult your healthcare provider if you suspect you have been exposed to or infected with mpox.
Read more: How Mpox Virus Spreads
1 year ago
How Mpox Virus Spreads
Mpox, previously known as monkeypox, is a viral infection that has grabbed global attention due to its increasing spread and impact on public health. This virus is part of the same family as smallpox but is generally less severe. Let’s explore the various ways mpox can be transmitted from one individual to another.
Direct Human-to-Human Transmission
Close or Intimate Contact
One of the primary ways mpox spreads is through close or intimate contact with an infected individual. The virus can be transmitted through direct skin-to-skin contact with the rash, scabs, or bodily fluids of someone who has mpox.
This contact can occur during various forms of intimate activities, including sex, kissing, or hugging.
Pregnant individuals who contract mpox can also pass the virus to their fetus during pregnancy or to their newborn during and after birth. Additionally, prolonged face-to-face interactions, such as talking or breathing in close proximity to an infected person, can also facilitate the spread of the virus through respiratory secretions, including saliva, snot, and mucus.
Read more: What is Mpox? How does it affect people?
Touching Contaminated Objects and Surfaces
Another significant mode of transmission for mpox is through contact with objects, fabrics, and surfaces that have been contaminated by an infected person. This includes items like clothing, bedding, and towels that have not been properly disinfected.
The virus can survive on these surfaces for extended periods, making it easy for someone else to contract the virus by touching these contaminated items.
Respiratory Droplets
While close physical contact is the most common way mpox spreads, the virus can also be transmitted through respiratory droplets. During face-to-face interactions, especially over a prolonged period, the virus can be expelled into the air through coughing, sneezing, or even talking.
These droplets can then be inhaled by another person, leading to infection. However, it is important to note that the risk of transmission through respiratory droplets is lower compared to direct skin-to-skin contact.
Sexual Transmission
The mpox virus can be transmitted through sexual activity. Democratic Republic of Congo (DRC) has had some cases where mpox transmission was linked with sexual contact, highlighting the importance of safe sexual practices in preventing the spread of mpox.
Read more: Mpox: Common Signs and Symptoms
Animal-to-Human Transmission
Contact with Infected Animals
Mpox is a zoonotic virus, meaning it can spread from animals to humans. The virus is endemic in certain regions of West and Central Africa, where it is naturally found in small wild animals, including rodents and primates.
Humans can contract the virus through direct contact with these infected animals, their fluids, or waste. Activities such as hunting, trapping, or processing wild animals in these regions pose a higher risk of contracting mpox.
1 year ago
Bangladeshi traveling from Qatar suspected of Mpox tests negative
A passenger suspected of having mpox (monkeypox) at Dhaka’s Hazrat Shahjalal International Airport upon landing on Friday (August 23, 2024) has tested negative today.
The passenger, hailing from Cumilla, arrived in Dhaka on August 23 at 9:20 am aboard a Qatar Airways flight. Upon arrival, airport health services flagged him as a potential mpox case due to his symptoms.
Read more: Mpox: Common Signs and Symptoms
The man was immediately transported by ambulance to the Infectious Diseases Hospital in Mohakhali. Dhaka for further examination. Dr. Ariful Bashar of the hospital confirmed that the patient was being tested and promised to provide further information once results were available.
Today, tests confirmed that the man does not have mpox, easing concerns raised by the initial diagnosis.
Read more: What is Mpox? How does it affect people?
1 year ago
Mpox: Common Signs and Symptoms
Mpox or Monkeypox has become a global concern over the last two years since its outbreak in the Democratic Republic of the Congo in 2022. Mpox has so far crossed the boundary of Africa and made its way through Europe to Asia. To ensure the prevention of this viral disease, mass awareness is a must. Let’s take a look into the early symptoms, rash progression, risk factors, incubation period, and contagious duration of the Monkeypox disease.
Major Signs and Symptoms of Mpox
In the early stages of sickness, people affected by Mpox will simply feel unwell. They will be seemingly showing “flu-like” symptoms. Most people will only suffer from these mild symptoms and recover within a period of 2 to 4 weeks.
Early Symptoms
Early symptoms of Mpox include:
Fever: A fever is often one of the first symptoms to appear when someone is infected with Mpox. The body’s temperature rises as a natural defense mechanism to help fight off the virus. This increase in temperature can range from a mild elevation to a high fever, often making the person feel very uncomfortable. The fever may come and go in waves and can be accompanied by a few other symptoms.
Read more: Pakistan's health ministry confirms a case of mpox but more tests are being done for its variant
Headache: Alongside fever, headaches are a common early symptom of Monkeypox. These headaches can vary in intensity, ranging from mild discomfort to severe pain. The headaches are usually persistent and can make concentration and everyday activities difficult.
Chills: Chills are often experienced as sudden, involuntary muscle contractions that result in shivering. This symptom usually accompanies the fever and can make a person feel cold even when the body temperature is elevated. Chills are a response to the body’s effort to raise its core temperature to fight the infection.
Joint Pains: Joint pains, also known as arthralgia, are common in the early stages of Monkeypox. This discomfort can affect any joint of the body, including the knees, elbows, wrists, and fingers. Joint pain can range from mild to severe and may be constant or intermittent. It often leads to stiffness and difficulty in movement, contributing to the overall feeling of malaise.
Read more: Congo's humanitarian crisis helped mpox spiral again into a global health emergency
Backache: Backache is another frequent symptom, often adding to the discomfort experienced during the early stages of Mpox. The pain is usually centered in the lower back but can also radiate to other areas. This pain can be persistent and may worsen with physical activity or prolonged sitting.
Muscle Aches: Muscle aches, or myalgia, are common and can affect various parts of the body. These aches can range from dull, persistent pain to more intense discomfort that limits movement. Muscle aches can affect the entire body or be localized to specific areas, making physical activities challenging and contributing to the overall sense of fatigue.
Swollen Lymph Nodes: Swollen lymph nodes, also known as lymphadenopathy, are a key indicator of Monkeypox infection. The lymph nodes, particularly those in the neck, armpits, and groin, may become tender and noticeably enlarged. This swelling occurs as the body’s immune system ramps up its response to fight the virus.
Read more: Health ministry issues mpox alert: Vigilance at entry points; no cases detected in Bangladesh yet
Extreme Tiredness: Extreme tiredness, or fatigue, is one of the most debilitating symptoms of Mpox. This profound exhaustion goes beyond normal tiredness, leaving individuals feeling drained and unable to perform everyday tasks. Fatigue can persist throughout the illness, even when other symptoms begin to improve.
1 year ago
What is Mpox? How does it affect people?
On August 14, The World Health Organization (WHO) declared Mpox or Monkeypox as a public health emergency of international concern, which is the highest alert the organization can decree. Since its earlier detection in the Democratic Republic of Congo in 2022, Mpox has been spreading across continents contaminating and killing thousands of people.
Recently, this deadly disease has been detected in Pakistan, sprouting fear in the neighboring South Asian countries. To stay safe, mass awareness should be raised against Mpox.
What is Mpox or Monkeypox?
Mpox or Monkeypox is a disease caused by the Mpox virus. When infected by this virus, people show symptoms similar to those of smallpox, like rashes, discolored and swollen lymph nodes, headache, muscle aches, fever, and so on.
Read more: Health ministry issues mpox alert: Vigilance at entry points; no cases detected in Bangladesh yet
Quite rare in humans, the Mpox virus mostly affects rodents, like rats, and mice, and primates, like gorillas, and monkeys. However, for the last two years, a new variation has been alarmingly raising concerns about infecting humans and causing deaths.
Mpox Variations
Till now, only two variations of the Mpox virus have been found liable for human illness—Clade I and Clade II. According to researchers, the variations liable for the recent outbreak and the outbreak in 2022 are different.
The global outbreak of 2022 that infected around 100,000 people was caused by the Clade II variation, whereas, Clade I is liable for the recent situation. The two mutant types share a few differences in terms of their ways of transmission, and symptoms.
Read more: How to Keep Your Skin Healthy During Monsoon
Clade I
Clade I shows a pattern in its process of transmission, taking advantage of a person’s immunodeficiency, making them weak, and slowly pushing them towards death. The mortality rate among the Clade I victims ranges from 1% to 10%.
As per reports, the victims have been mostly the inhabitants of Congo. However, the number of victims went up due to the rapid contamination among people in other areas of the world. Clade I is more frequent among children who are infected through contact with animals or other members of their families.
Clade II
Clade II is responsible for the 2022 outbreak of Mpox. The death rate of Clade II is low, counting only 1% to 4%. The severity of the illness is also more tolerable, causing rashes on a random part of the body mostly around the face and torso instead of the full body.
Read more: Congo's humanitarian crisis helped mpox spiral again into a global health emergency
How Did the Recent Variation of Mpox Spread?
The transmission pathways of Mpox are diverse, including close personal contact, contact with contaminated materials, and interaction with infected animals. Clade II, has shown unique patterns of spread, which has raised new concerns and challenges for public health efforts. Here are some common modes of Transmission of Mpox virus.
Close Personal Contact
The primary mode of Mpox transmission is through close, personal contact with an infected individual. This includes direct skin-to-skin contact with an infected person’s rashes, scabs, or bodily fluids.
The virus can also spread through contact with respiratory secretions such as saliva or mucus. Intimate activities, such as sex, as well as prolonged face-to-face interactions, can facilitate the transmission of the virus.
Read more: Pakistan's health ministry confirms a case of mpox but more tests are being done for its variant
In the 2022 global outbreak of Clade IIb, the virus predominantly spread through sexual contact. This pattern of transmission underscores the importance of targeted public health messaging and interventions to prevent the further spread of the virus in at-risk populations.
Contact with Contaminated Materials
Mpox can also spread through contact with objects, fabrics, and surfaces that have been contaminated by an infected person. Items like bedding, towels, clothing can harbor the virus if they are not properly disinfected.
This mode of transmission highlights the importance of maintaining good hygiene practices and ensuring that environments, where infected individuals have been, are thoroughly cleaned and disinfected.
Read more: Comprehensive Guide to the Best Home Fitness Equipment in Bangladesh for 2024
Animal-to-Human Transmission
Another significant route of Monkeypox transmission is through contact with infected animals. Mpox is endemic in certain wild animals in West and Central Africa, particularly rodents. People can contract the virus by hunting, trapping, or processing these animals, or through bites, scratches, or direct contact with an infected animal’s fluids or waste.
While the risk of transmission from pets is low, close contact with an infected pet, such as petting, cuddling, or sharing sleeping spaces, could potentially spread the virus to humans.
Recent Developments in Mpox Spread
In recent outbreaks, particularly in the Democratic Republic of Congo, the Clade I variant of the Mpox virus has shown an alarming trend of spreading through sexual contact.
Read more: Circadian Rhythm: How to Reset the Biological Master Clock
Moreover, early evidence indicates that Clade I might possess certain properties that enhance its ability to spread from person to person more easily. This has raised concerns about the potential for more widespread outbreaks, particularly in regions with limited surveillance and healthcare infrastructure.
Conclusion
The recent variations of Mpox, particularly Clade II and Clade I, have shown concerning patterns of transmission.
The virus's ability to spread through close personal contact, contaminated materials, and interaction with infected animals highlights the importance of public awareness and targeted health interventions.
Read more: Cerebral Haemorrhage: Signs, Reasons, Treatment, and Prevention
As the situation evolves, understanding the transmission pathways of Mpox or Monkeypox is essential for controlling the spread and protecting vulnerable populations.
1 year ago
1st Monkeypox death in US confirmed by LA County health officials
A Los Angeles County resident with a compromised immune system has died from monkeypox, local health officials announced Monday. It's believed to be the first U.S. fatality from the disease.
The Los Angeles County Department of Public Health announced the cause of death, and a spokesperson said it was confirmed by an autopsy. The patient was severely immunocompromised and had been hospitalized. No other information on the person was released.
The Centers for Disease Control and Prevention tracks cases and has not confirmed any U.S. deaths from the disease. LA County officials say they worked with the CDC on their case.
Also read: US may expand monkeypox vaccine eligibility to men with HIV
A CDC spokesperson confirmed the cooperation but did not immediately respond when asked if this was the first U.S. death.
Texas public health officials on Aug. 30 reported the death of a person who had been diagnosed with monkeypox. The person was severely immunocompromised and their case is under investigation to determine what role monkeypox may have played in their death.
Monkeypox is spread through close skin-to-skin contact and prolonged exposure to respiratory droplets. It can cause a rash, fever, body aches and chills. Relatively few people require hospitalizations and only a handful of deaths worldwide have been directly linked to the disease.
Also read: WHO: Monkeypox cases drop 21%, reversing month-long increase
The CDC recommends the monkeypox vaccine for people who are a close contact of someone who has disease; people who know a sexual partner was diagnosed in the past two weeks; and gay or bisexual men who had multiple sexual partners in the last two weeks in an area with known virus spread. Shots are also recommended for health care workers at high risk of exposure.
Also read: WHO: Monkeypox cases drop 21%, reversing month-long increase
The United States has the most cases globally, with 21,985 confirmed, according to the CDC. California has recorded the most cases nationally, with more than 4,300. Black people and Latinos have been disproportionately infected.
A recent decline in cases, combined with an uptick in vaccinations, has encouraged the White House as officials promise to ramp up vaccination offerings at LGBTQ Pride festivals around the country in the coming weeks.
3 years ago
US may expand monkeypox vaccine eligibility to men with HIV
U.S. officials are considering broadening recommendations for who gets vaccinated against monkeypox, possibly to include many men with HIV or those recently diagnosed with other sexually transmitted diseases.
Driving the discussion is a study released Thursday showing that a higher-than-expected share of monkeypox infections are in people with other sexually transmitted infections.
Dr. John T. Brooks, chief medical officer for the Centers for Disease Control and Prevention's monkeypox outbreak response, said the report represents a “call to action.”
Brooks told The Associated Press on Thursday that he expected vaccine recommendations to expand and that "the White House, together with CDC, are working on a plan for what that will look like.”
Also read: WHO: Monkeypox cases drop 21%, reversing month-long increase
Currently, the CDC recommends the vaccine to people who are a close contact of someone who has monkeypox; people who know a sexual partner was diagnosed in the past two weeks; and gay or bisexual men who had multiple sexual partners in the last two weeks in an area with known virus spread.
Shots are also recommended for health care workers at high risk of exposure.
The vast majority of monkeypox cases are in men who have sex with men who reported close contact with an infected person during sex. But the new CDC report suggested infections in people with HIV and other STDs may be a bigger issue then previously realized.
The report looked at about 2,000 monkeypox cases from four states and four cities from mid-May to late July.
It found 38% of those with monkeypox infections had been diagnosed with HIV, far higher than their share of the population among men who have sex with men.
Also read: Public health emergency declared over monkeypox in WA county
The study also found that 41% of monkeypox patients had been diagnosed with an STD in the preceding year. And about 10% of those patients had been diagnosed with three or more different STDs in the prior year.
There were racial differences. More than 60% of Black Americans with monkeypox had HIV, compared with 41% of Hispanic people, 28% of whites and 22% of Asians.
Jason Farley, an infectious disease expert at the Johns Hopkins School of Nursing, said men of color who have sex with men should be at the front of the line for monkeypox vaccine doses. Within those racial and ethnic groups, the next priority should be anyone living with HIV or was recently diagnosed with a STD, he said.
The study has several limitations, including that the data may not be nationally representative, the authors said.
Brooks said the findings could lead to vaccines being recommended for people with recent STD infections, people with HIV, people taking pre-exposure prophylaxis (PrEP) medications to prevent HIV infection and, possibly, prostitutes.
Discussions of expanding eligibility will have to take into account supply of the two-dose vaccine. And any substantial expansion of monkeypox vaccination recommendations may also be subject to review by CDC’s outside vaccine advisers, health officials say.
Also on Thursday, the CDC sent a letter to state and local health departments that said federal funds for HIV and STD prevention can also now be used against monkeypox. Cases in the U.S. seem to be declining, officials say.
3 years ago
WHO: Monkeypox cases drop 21%, reversing month-long increase
The number of monkeypox cases reported globally dropped by 21% in the last week, reversing a month-long trend of rising infections and a possible signal the outbreak in Europe may be starting to decline, according to a World Health Organization report issued Thursday.
The U.N. health agency reported 5,907 new weekly cases and said two countries, Iran and Indonesia, reported their first cases. To date, more than 45,000 cases have been reported in 98 countries since late April.
Cases in the Americas accounted for 60% of cases in the past month, WHO said, while cases in Europe comprised about 38%. It said infections in the Americas showed “a continuing steep rise.”
The Africa Centers for Disease Control and Prevention said Thursday the continent had 219 new cases reported in the past week, a jump of 54%. Most were in Nigeria and Congo, the agency said.
Also read: Public health emergency declared over monkeypox in WA county
In early July, just weeks before the agency declared the international spread of the disease to be a global emergency, WHO’s Europe director said countries in the region were responsible for 90% of all laboratory confirmed cases of monkeypox.
British health authorities said last week after seeing a decline in the number of new cases getting reported daily that there were “early signs” the country’s monkeypox outbreak was slowing.
The U.K.’s Health Security Agency downgraded the country’s monkeypox outbreak last month, saying there was no evidence the once rare disease was spreading beyond men who were gay, bisexual or had sex with other men.
Since monkeypox outbreaks in Europe and North America were identified in May, WHO and other health agencies have noted that its spread was almost exclusively in men who have sex with men.
Also read: Monkeypox cases cross 35,000: WHO
Monkeypox has been endemic in parts of Africa for decades and experts suspect the outbreaks in Europe and North America were triggered after the disease started spreading via sex at two raves in Spain and Belgium.
WHO’s latest report said 98% of cases are in men and of those who reported sexual orientation, 96% are in men who have sex with men.
“Of all reported types of transmission, a sexual encounter was reported most commonly,” WHO said. “The majority of cases were likely exposed in a party with sexual contacts,” the agency said.
Among the monkeypox cases in which the HIV status of patients was known, 45% were infected with HIV.
WHO has recommended that men at high risk of the disease temporarily consider reducing their number of sex partners or refrain from group or anonymous sex.
Monkeypox typically requires skin-to-skin or skin-to-mouth contact with an infected patient’s lesions to spread. People can also become infected through contact with the clothing or bedsheets of someone who has monkeypox lesions.
With globally limited vaccine supplies, authorities in the U.S., Europe and the U.K. have all begun rationing doses to stretch supplies by up to five times.
WHO has advised countries that have vaccines to prioritize immunization for those at high risk of the disease, including gay and bisexual men with multiple sex partners, and for health workers, laboratory staff and outbreak responders.
While Africa has reported the most suspected deaths from monkeypox, the continent has no vaccine supplies apart from a very small stock being tested in a research study in Congo.
“As we know, the situation with monkeypox vaccine access is very topical, but there are not enough doses of vaccines," Nigeria Center for Disease Control Director-General Ifedayo Adetifa said this week. Potentially, a lot more more doses will become available, but because of challenges with manufacturing factories and unexpected uptick in monkeypox cases, the vaccine may actually not be available until 2023.”
3 years ago
US declares public health emergency over monkeypox outbreak
The federal government declared a public health emergency Thursday to bolster the response to the monkeypoxoutbreak that has infected more than 7,100 Americans.
The announcement will free up money and other resources to fight the virus, which may cause fever, body aches, chills, fatigue and pimple-like bumps on many parts of the body.
“We are prepared to take our response to the next level in addressing this virus, and we urge every American to take monkeypox seriously,” said Xavier Becerra, head of the U.S. Department of Health and Human Services.
The declaration by HHS comes as the Biden administration has faced criticism over monkeypox vaccine availability. Clinics in major cities such as New York and San Francisco say they haven’t received enough of the two-shot vaccine to meet demand, and some have had to stop offering the second dose to ensure supply of first doses.
The White House said it has made more than 1.1 million doses available and has helped to boost domestic diagnostic capacity to 80,000 tests per week.
The monkeypox virus spreads through prolonged skin-to-skin contact, including hugging, cuddling and kissing, as well as sharing bedding, towels and clothing. The people who have gotten sick so far have been primarily men who have sex with men. But health officials emphasize that the virus can infect anyone.
No one in the United States has died. A few deaths have been reported in other countries.
Read: China cannot stop US officials from visiting Taiwan: Pelosi
Earlier this week, the Biden administration named top officials from the Federal Emergency Management Agency and the Centers for Disease Control and Prevention to serve as the White House coordinators to combat monkeypox.
Thursday’s declaration is an important — and overdue — step, said Lawrence Gostin, a public health law expert at Georgetown University.
“It signals the U.S. government’s seriousness and purpose, and sounds a global alarm,” he said.
Under the declaration, HHS can draw from emergency funds, hire or reassign staff to deal with the outbreak and take other steps to control the virus.
For example, the announcement should help the federal government to seek more information from state and local health officials about who is becoming infected and who is being vaccinated. That information can be used to better understand how the outbreak is unfolding and how well the vaccine works.
Gostin said the U.S. government has been too cautious and should have declared a nationwide emergency earlier. Public health measures to control outbreaks have increasingly faced legal challenges in recent years, but Gostin didn’t expect that to happen with monkeypox.
“It is a textbook case of a public health emergency,” Gostin said. “It’s not a red or a blue state issue. There is no political opposition to fighting monkeypox.”
A public health emergency can be extended, similar to what happened during the COVID-19 pandemic, he noted.
The urgency in the current response stems from the rapid spread of the virus coupled with the limited availability of the two-dose vaccine called Jynneos, which is considered the main medical weapon against the disease.
3 years ago
Brazil confirms first monkeypox-related death
Brazil on Friday confirmed the country's first monkeypox-related death, according to the Health Ministry.
The case was reported in Belo Horizonte, capital of the southeast Minas Gerais state, and the victim was a 41-year-old man who was undergoing treatment for other serious clinical conditions, including cancer, and whose health deteriorated after getting infected, the ministry said.
The man, whose name was not released, was admitted to a public hospital in Belo Horizonte, where he suffered septic shock aggravated by monkeypox.
Read: New York City declares monkeypox a public health emergency
In Minas Gerais, state health authorities said there were 44 confirmed cases of the disease and 130 suspected cases under investigation.
In Brazil, there were 978 confirmed cases of monkeypox as of Wednesday.
The World Health Organization has declared the current outbreak a public health emergency of international concern.
Experts classify monkeypox as a rare viral disease that causes skin lesions and is transmitted through close contact with an infected person, including through hugs, kisses, massages or sexual intercourse, in addition to being transmitted through respiratory secretions or contact with clothing, towels, or other items used by the infected person. ■
3 years ago






.jpg)









