Hormone therapy can ease menopause symptoms such as hot flashes, night sweats and sleep problems, but doctors say women should understand both its benefits and risks before deciding on treatment.
The issue was highlighted during a recent U.S. Food and Drug Administration (FDA) expert panel review, which debated whether health warnings on some hormone medications should be changed.
Hormone therapy was once widely prescribed, but its use dropped sharply in 2002 when a large federal study linked one type to higher risks of breast cancer and blood clots. Later research, however, found that today’s treatments are safer and can be a good option for many women.
“There is still a lot of confusion and a lot of fear,” said Grayson Leverenz, 50, of North Carolina, who hesitated to take hormones but said the therapy ultimately helped her sleep, eased her pain and reduced anxiety.
How hormone therapy works
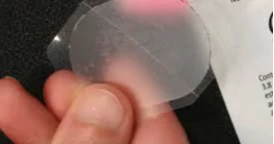
Systemic treatments — delivered through pills, patches, gels, sprays or vaginal rings — raise hormone levels enough to relieve hot flashes and other widespread symptoms. Localized, low-dose vaginal estrogen is considered lower risk and is mainly used for dryness.
The Menopause Society notes that starting hormone therapy within 10 years of menopause may also protect heart health, maintain bone density and lower the risk of diabetes.
Risks and limits
Doctors stress that age, medical history and length of treatment matter. Estrogen-only therapy can usually be used for up to seven years, and combined estrogen-progestogen therapy for three to five years, before breast cancer risk increases.
Hatchlings of 100-year-old tortoise parents unveiled at Philadelphia Zoo
Both types raise the risk of stroke, though the risk declines after stopping treatment. Oral medications also raise the risk of blood clots, but patches, gels or sprays may carry less risk.
“A lot of these risks are small,” said Dr. Nanette Santoro of the University of Colorado. “They have to be weighed against the benefit of symptom relief.”
Regulatory debate
All estrogen drugs currently carry “black box” warnings about stroke, blood clots and cognitive risks. Some FDA panelists suggested those warnings could be relaxed, but more than 70 experts have urged caution, warning that premature changes could mislead patients.
Alternatives
New non-hormonal options such as fezolinetant (Veozah) can relieve hot flashes and night sweats. Gabapentin, an anti-epileptic drug, is sometimes used at low doses, while moisturizers and lifestyle changes like exercise and diet can also help.
Doctors caution women against unproven supplements marketed as menopause cure-alls. “If it looks too good to be true, it probably is,” Santoro said.
Source: Agency